Note this forecast page is not the most recent forecast available.
View the most current forecast report
Researcher Analyzes Arizona COVID-19 Spread Models for Decision-Makers
The following information regarding the spread of COVID-19 in Arizona was prepared by Joe Gerald, MD, PhD, a researcher at the Mel and Enid Zuckerman College of Public Health (MEZCOPH) at the University of Arizona. This information has also been reviewed by other MEZCOPH faculty.
This data were obtained from the Arizona Department of Health Services COVID-19 webpage and reflect conditions in Arizona as of August 14, 2020.
This information is intended to help guide our response to the outbreak. It is not intended to predict how this pandemic will evolve. Rather, this model extrapolates what might occur if current conditions remain unchanged. As regional authorities and healthcare providers respond, their actions are expected to mitigate the worst consequences of this pandemic.
COVID-19 Disease Outbreak Forecast
Arizona State and Pima County
Updated August 14, 2020
Disclaimer: This information represents my personal views and not those of The University of Arizona, the Zuckerman College of Public Health, or any other government entity. Any opinions, forecasts, or recommendations should be considered in conjunction with other corroborating and conflicting data. Updates can be accessed at https://publichealth.arizona.edu/news/2020/covid-19-forecast-model.
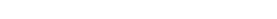
For the week ending August 9th, 5322 new Covid-19 cases were diagnosed in Arizona (Figure 1). However, this tally likely undercounts the actual number of new cases owing to persistent, but diminishing, reporting delays. For example, last week’s tally has been upwardly revised by 15% from 7006 to 8120 cases (a 40% smaller revision than last week) and the case count from two weeks ago was revised by 2% (an 80% smaller revision than last week). Despite some minor testing concerns, case counts demonstrate viral transmission is rapidly waning from its late-June peak.
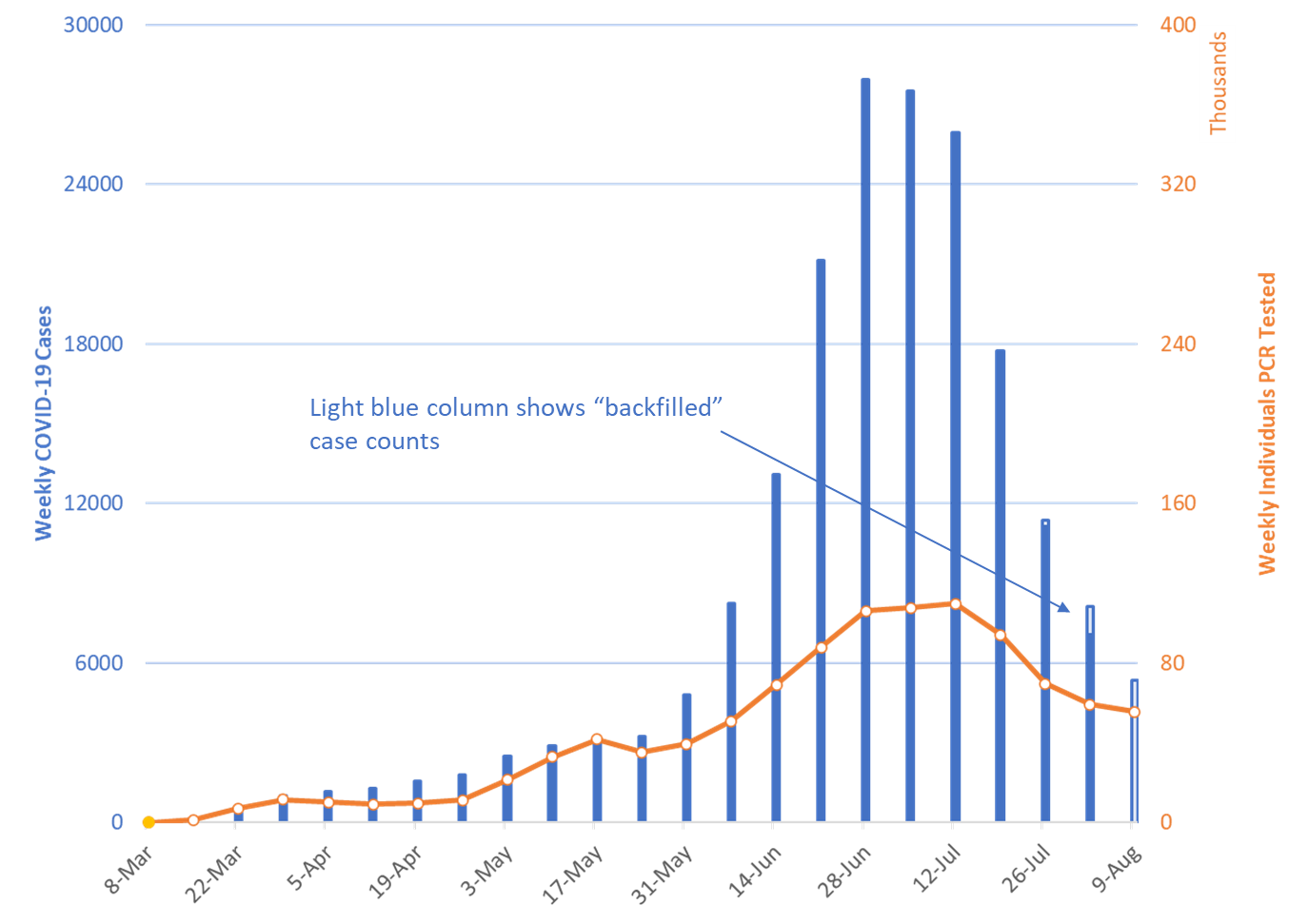
The percent of patients testing positive has declined from a peak of 23% the week ending July 25th to 9% the week ending August 9th (Figure 2 following page). A declining test positive percentage in the face of declining testing supports slowing viral transmission. The percent of patients testing positive on the antibody (serology) test has remained steady at approximately 13%.
| Figure 1. Newly Diagnosed Covid-19 Cases in Arizona and Number of Individuals Undergoing PCR Testing March 1 through August 9. |
Recent controversy has arisen regarding how ADHS calculates the PCR test + percentage. In brief, not all negative tests are reported to ADHS; therefore, ADHS has decided to calculate the test + percentage on only electronically reported tests which account for roughly 75-80% of cases. This is because electronically reported labs include positive and negative results. If systematic differences exist between reporting and non-reporting labs or the patients they serve, then the ADHS calculation could be biased. Nonetheless, I support the ADHS decision and use the same approach. Johns Hopkins uses the following: cases / cases + reported negatives. This approach upwardly biases the result so can be used as a upper bound.
| Figure 2. Weekly Number Patients Tested and Percent of Individuals with Positive Covid-19 PCR and Serology Results March 1 - August 9. |
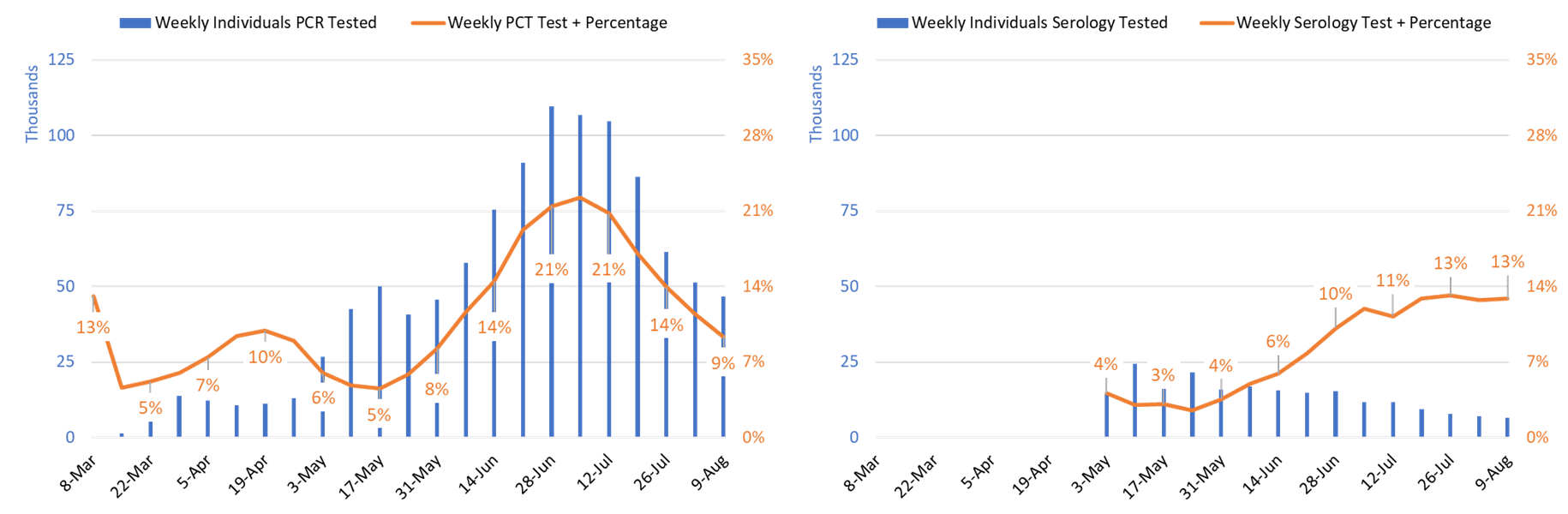
Reporting lag for PCR test results has been shortening since the week ending July 19th. The week ending August 2nd saw 75% of results being reported within 48 hours of test collection. Assuming adequate case investigation and contact tracing resources, this turn-around is sufficiently fast to enable an effective public health response. Unfortunately, there are no publicly available metrics to gauge the rapidity of contact tracing or adherence with isolation requirements.
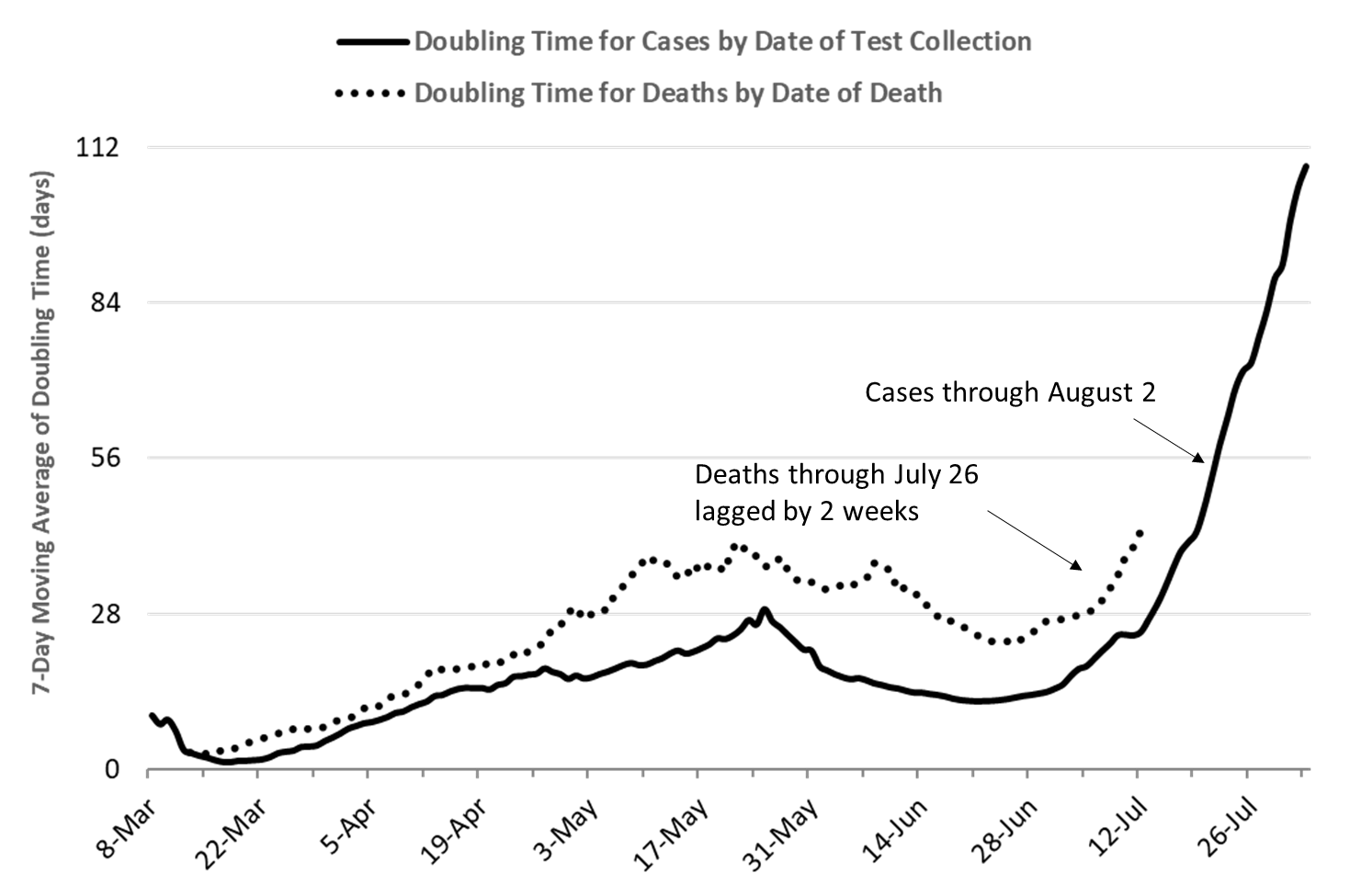
The 7-day moving average of doubling time for cumulative Covid-19 cases shortened from a peak of 29 days on May 25th to a trough of 12 days on June 21st (Figure 3, following page). As of August 2nd, it was 109 days. Because the testing lag has shortened, I am now displaying new case data through August 2nd (only lagged a week). The sharply lengthening doubling is consistent with the rapidly declining case counts. The doubling time for cumulative deaths has shortened from a high-water mark of 41 days on June 5th to a trough of 23 days on July 10th. As of July 26th, it was 43 days. The pace of Covid-19 deaths is now clearly slowing. Given conditions are steadily improving, I am going to retire this graph until conditions materially change.
| Figure 3. 7-Day Moving Average of Doubling Time of Cumulative Cases through August 2 Superimposed on Lagged (2-week) Doubling Time of Cumulative Deaths through July 26. |
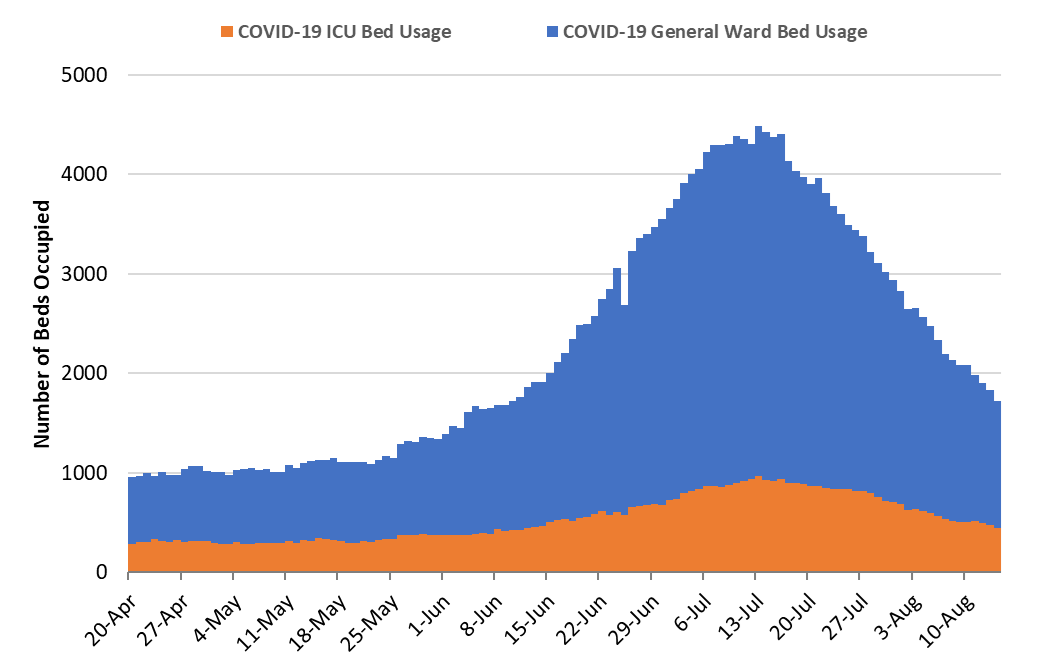
| Figure 4. Arizona Daily Covid-19 General Ward and ICU Census April 20 – August 14. |
As of August 14, Covid-related hospitalizations remain 58% higher than a May 22 plateau, 1724 versus 1093 occupied beds (Figure 4). Since last week, Covid-19 hospitalization has decreased 22% from 2198 to 1724 occupied beds. Hospital occupancy should continue to decline over the coming weeks.
As of August 14th, 1282 (16%) of Arizona’s 8002 general ward beds were occupied by patients with suspected or confirmed Covid-19 infection, a 23% decline from last week. An additional 1346 (17%) beds remain available which is slightly lower than last week’s 1384 beds. Similarly, 442 (26%) of Arizona’s 1701 ICU beds were occupied for Covid-19 care, an 18% decrease from last week. An additional 370 beds (22%) beds remain available which is higher than last week’s 293 beds.
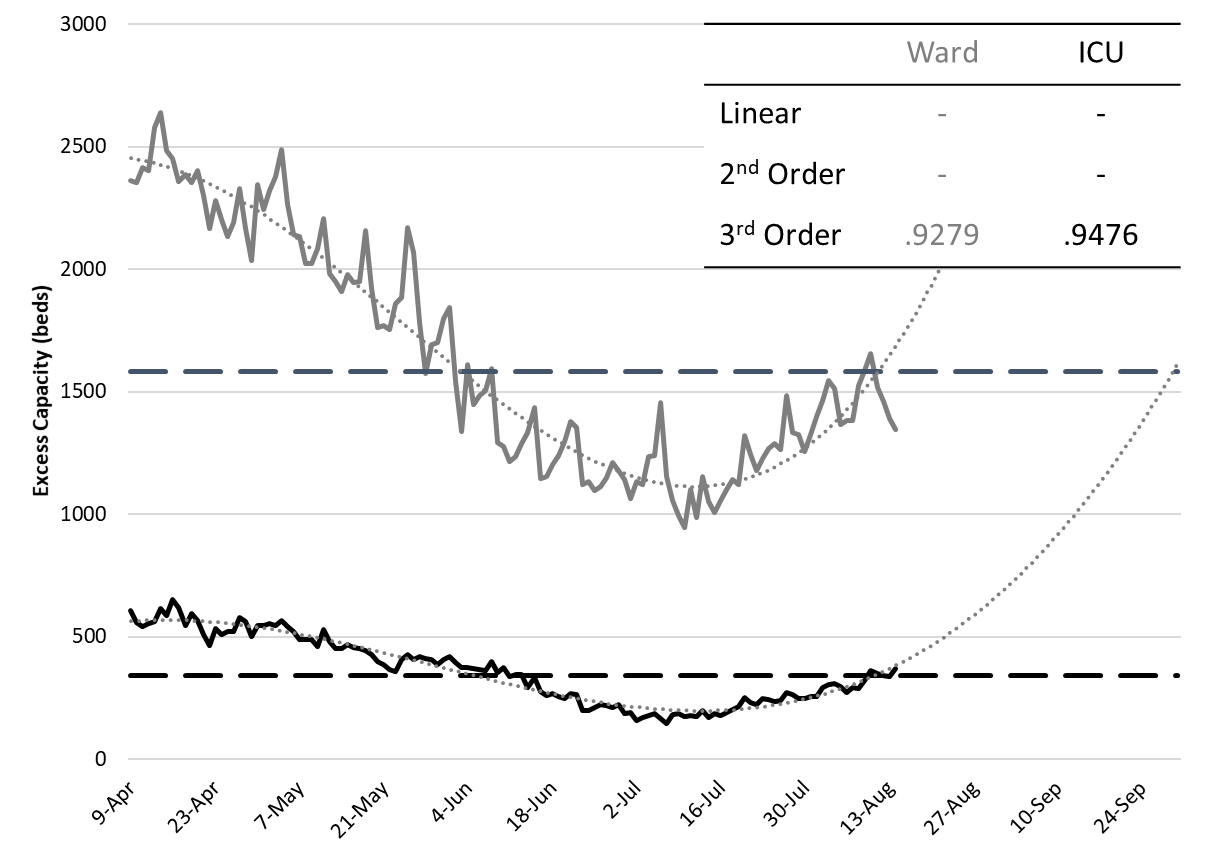
Arizona will not exceed its listed capacity of non-surge general ward or ICU beds unless improvements reverse (Figure 5, following page). In fact, state-wide occupancy has already begun to dip below the 80% threshold in general ward and ICU settings. Given that this threshold generally marks the point when hospitals invoke crisis care standards and/or delay elective procedures, this is welcomed news. Many non-Covid patients now have access to needed care; however, continued vigilance is needed to ensure the backlog of care has time to resolve.
| Figure 5. Observed and Projected Excess Non-Surge General Ward and ICU Capacity April 20 – September 31. |
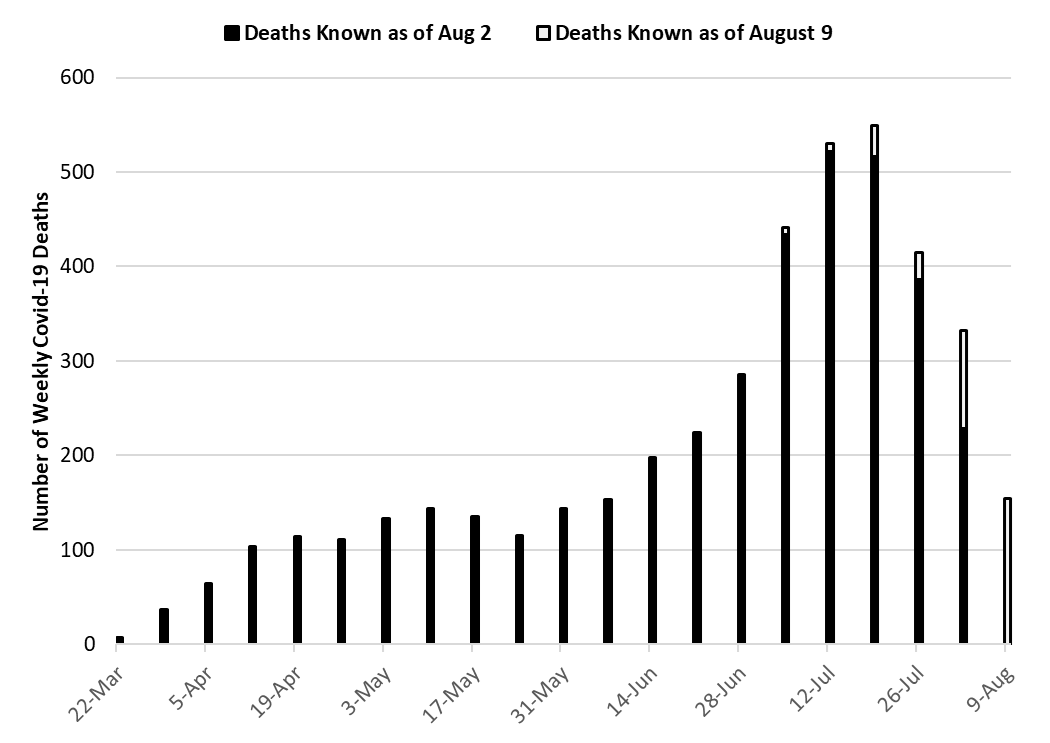
| Figure 6. Weekly Arizona Covid-19 Deaths March 1 – August 9 by Date of Death |
With 549 deaths reported to date, the week ending July 19th has overtaken the week ending July 12th as Arizona’s deadliest month (Figure 6). However, “only” 415 deaths have been reported for the week ending July 26th suggesting that it is unlikely to set a new record as additional deaths are reported.
As mentioned previously, the doubling time for cumulative deaths is now lengthening indicating that a peak in weekly deaths is likely to be readily identifiable soon. This would be a welcomed reprieve and a sure indicator that sustained progress has been made.
Pima County Outlook
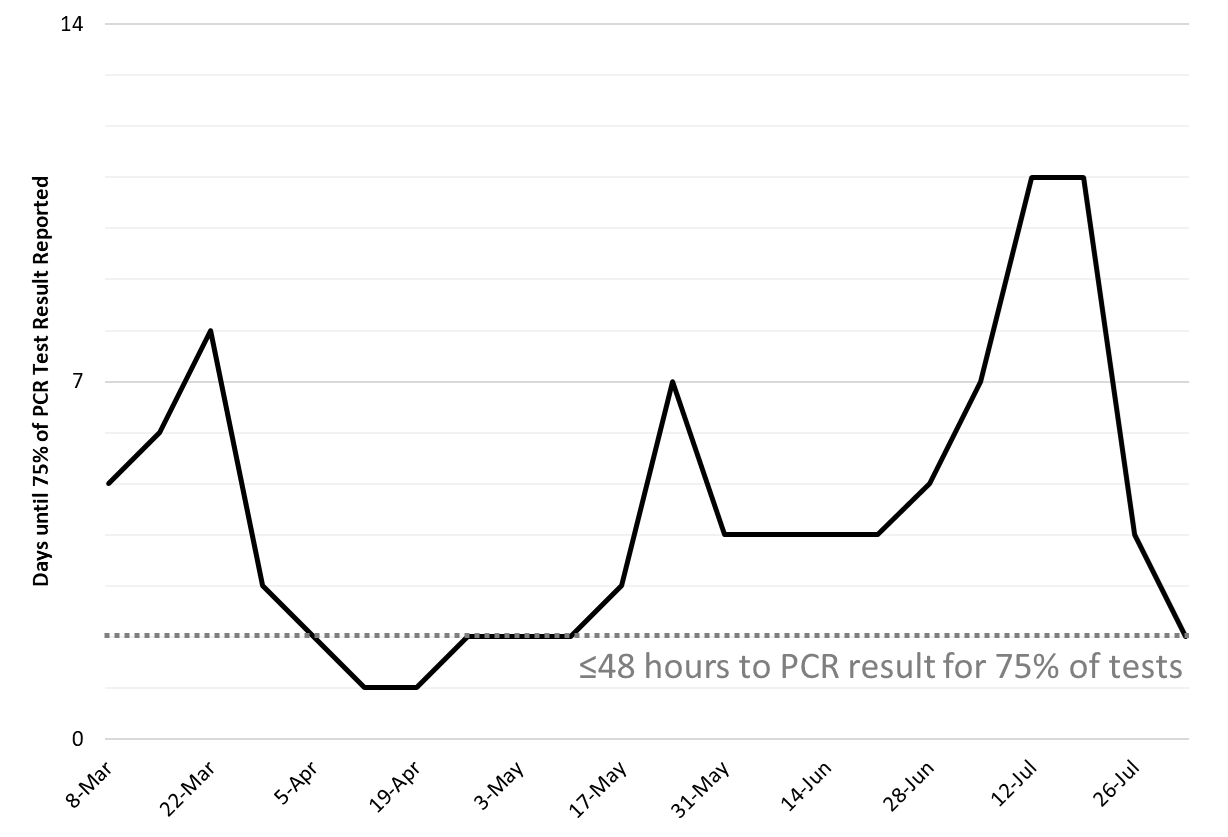
For the week ending August 9th, 799 Pima County residents were diagnosed with Covid-19. Unlike the state-wide figures, this count is less certain given an unexpectedly large “backfill” event for the week ending August 2nd. That week’s count of 874 cases has since been upwardly revised by 63% to 1423 cases this week (Figure 7). The preceding week was upwardly revised by a smaller 9%. While the pace of new case counts is substantially lower than the early July peak, the exact amount of decline remains a bit muddled in Pima County. Continued attention to this unusual activity is warranted.
| Figure 7. Newly Diagnosed Covid-19 Cases in Pima County and Individuals PCR Tested through August 9. |
Summary:
- The pace of viral transmission continues to slow appreciably as indicated by declining case counts and hospital utilization. Deaths likely peaked the week ending July 26th.
- Reporting lag for PCR results is improving making it easier to interpret changes in case counts and to conduct timely case identification, contact tracing, and isolation. This is mostly attributable to lower case counts as testing volume has been declining for the past several weeks.
- Absolute levels of community-driven viral transmission remain comparatively high as evidenced by large numbers of weekly Covid-19 cases, about twice as large as before the May 15th re-opening of Arizona’s economy.
- For most locales, government-mandated social distancing restrictions and mask-wearing will be needed for the foreseeable future to “claw back” excess hospital capacity, restore some of the lost safety margin, and address the backlog of patients waiting for “elective care.”
- Covid-related hospital utilization continues to decline while excess capacity is being replenished more slowly owing to larger amounts of non-Covid care. Adequate capacity is available for the foreseeable future. Personnel shortages and fatigue will still be problematic, especially in critical care settings.
- From now until January, non-Covid hospitalizations are expected to increase putting additional strain on hospital capacity. In addition, hospitals will be experiencing larger volumes of elective care to reduce the backlog of patients.
- Many ICUs will remain at or near capacity for the next several weeks due to long length-of-stays for many critically ill Covid-19 patients. Maintaining an adequate supply of health care workers will continue to be a challenge. Nevertheless, state-wide average hospital and ICU occupancy have dipped below 80% this past week which is an important milestone.
- Current Covid-19 test capacity is improving but remains inadequate to meet both clinical and public health demands as the test positive percentage is 9%, which is above the recommended 3 – 5%.
- Some controversy surrounds the “true” test positive rate owing to non-reported negative test results. To the extent that electronically reported tests are reflective of the larger population, this is not a critical problem. However, it may be exacerbated as antigen testing becomes more prevalent because negative antigen results are not routinely reported.
Analysis comparing Covid-19 case fatality rates between Pima and Maricopa Counties
This analysis compares Covid-19 mortality in Pima and Maricopa Counties. These data are current to August 6th, 2020. This report was initiated by the observation of a persistently higher crude case fatality rate in Pima County. This analysis should be interpreted cautiously as many confounding variables were unavailable and the analytic approach was rather rudimentary. Nonetheless, the results indicate that a substantial portion of the mortality differences between Maricopa and Pima Counties is attributable to differences in the age distribution of Covid-19 cases. The key finding is that Pima County’s distribution of recognized cases was skewed towards older residents who were at greater risk of death; this was particularly true of the outbreak prior to the mid-May re-opening of Arizona’s economy. Since that time, absolute and relative crude case fatality rates have converged as the populations most affected have become more similar in age.
As of August 6th, Arizona had recorded 185,053 Covid-19 cases and 4,081 deaths corresponding to a state-wide crude case fatality ratio (CFR) of 2.21% (Table 1). Similar tabulations indicate that Pima County’s crude CFR was 49% higher than Maricopa County’s, 2.75% versus 1.85%, respectively. However, when deaths are normalized by population size, Covid-19 mortality was in fact 12% higher in Maricopa County, 51.4 versus 46.0 deaths per 100,000 residents, respectively. Combined, these data suggest that the Covid-19 outbreak was more prevalent in Maricopa County, but the fatality rate was higher in Pima County. Note: Calculating the CFR using real-time data will skew rates downward as more recent cases remain at risk of future mortality.
Table 1. Covid-19 Cases, Deaths and Crude Case Fatality Ratio (CFR) for Arizona, Maricopa County and Pima County through August 6, 2020.
|
|
Cases |
Cases per 100,000* |
Deaths |
Deaths per 100,000 |
Crude CFR |
|
Arizona |
185,053 |
2,542 |
4,081 |
56.1 |
2.21% |
|
Maricopa County |
124,924 |
2,785 |
2,307 |
51.4 |
1.85% |
|
Pima County |
17,497 |
1,671 |
482 |
46.0 |
2.75% |
*The population estimate for Arizona, Maricopa County and Pima County is 7279000, 4485000, and 1047000, respectively. The crude CFR above understates the true CFR because some deaths have yet to occur among those recently diagnosed.
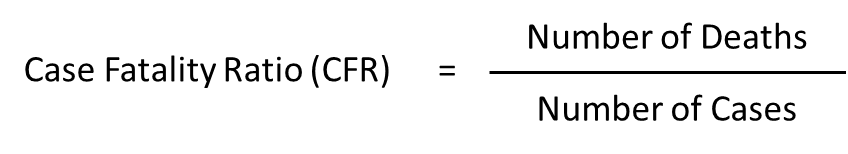
Several factors could distort the CFR calculations including differential testing capacity, age distributions, and health status among the respective counties. As a reminder, the crude CFR is a ratio measure with the number of Covid-19 deaths in the numerator and the number of Covid-19 cases in the denominator:
Given Arizona’s PCR testing woes, Maricopa County’s higher case count could have been attributable to more frequent testing rather than greater viral spread. On a per capita basis, PCR testing was 21% more prevalent in Maricopa County, 144 versus 119 tests per 100,000 residents, respectively. However, the population-normalized case rate was even higher than differential testing rates would suggest, 2785 versus 1671 cases per 100,000 residents, respectively, a 67% higher rate.
This differential between testing capacity and case counts is corroborated by a higher PCR test + percentage in Maricopa County than Pima County, 19% versus 14%, respectively. Taken together, these data indicate that testing capacity was more constrained in Maricopa County relative to the size of its outbreak. Therefore, greater viral spread is a better explanation of Maricopa County’s higher case count than more frequent testing.
Greater viral spread in Maricopa County is also corroborated by higher health care utilization rates. For example, hospitalization rates (966 versus 566 per 100,000 residents) and ICU admissions (477 versus 309 per 100,000 residents) were 71% and 54% more frequent in Maricopa County than Pima County (Figure 1 following page). Because these rates are thought to be somewhat intrinsic to Covid-19’s severity, higher per capita health care utilization in Maricopa County substantiates that its higher case count was not an artifact of testing but rather an indicator of more widespread viral transmission. If this was so, it begs the question why weren’t deaths more prevalent as well?
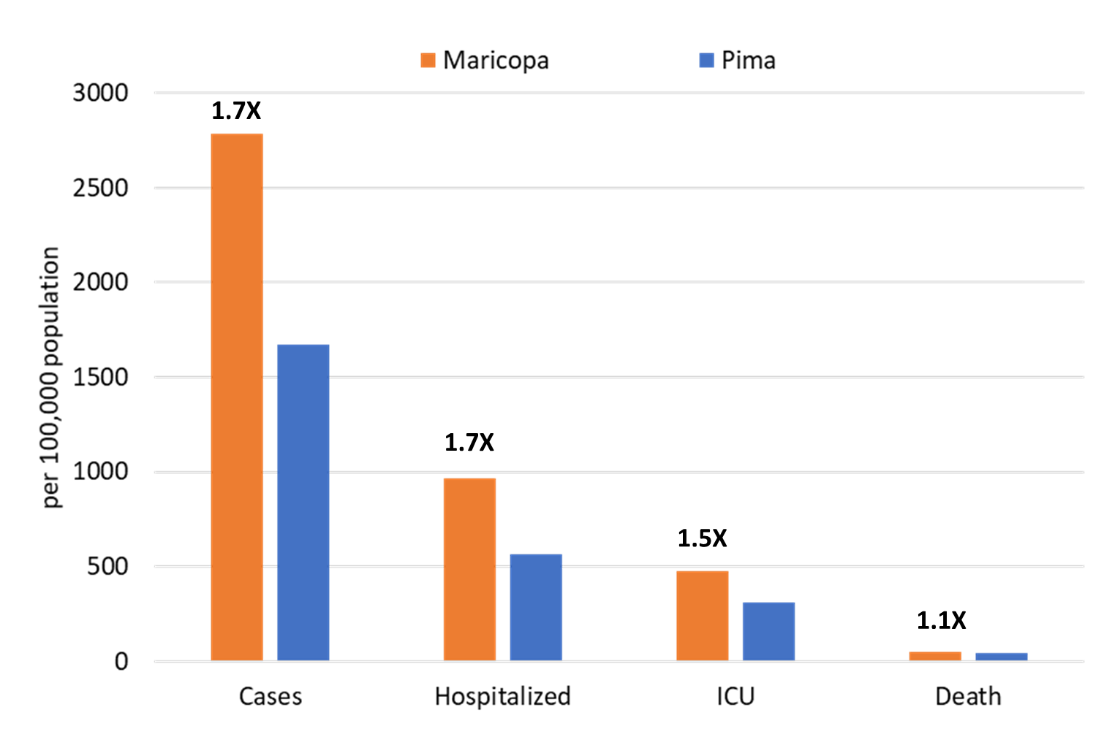
| Figure 1. Covid-19 Cases, Hospitalizations, ICU Admissions and Deaths in Maricopa County and Pima County through August 6, 2020. (These data are derived from completed case investigations and therefore may undercount actual health care utilization.) |
As of August 6, approximately 80% of all Arizona Covid-19 deaths have occurred among those 60+ years of age and about 40% have occurred among those 80+ years of age. Interestingly, this closely aligns with the distribution of non-Covid deaths in a typical year in Arizona. Because age is so strongly correlated with Covid-19 mortality, differences in the age distribution of Covid-19 cases between the two counties could explain some of the difference between their respective CFRs.
In fact, the age distribution was skewed between the two counties such that a higher proportion of Pima County’s cases were among those 60+ years of age, 18.9% versus 15.1%, respectively (Figure 2). Similarly, the proportion of cases among those 80+ years of age, those at highest risk of dying, was also higher, 4.3% versus 2.9%, respectively. Because the age distribution of cases differs between the two counties, it is reasonable to ask how much impact it might have had on observed differences in the CFRs.
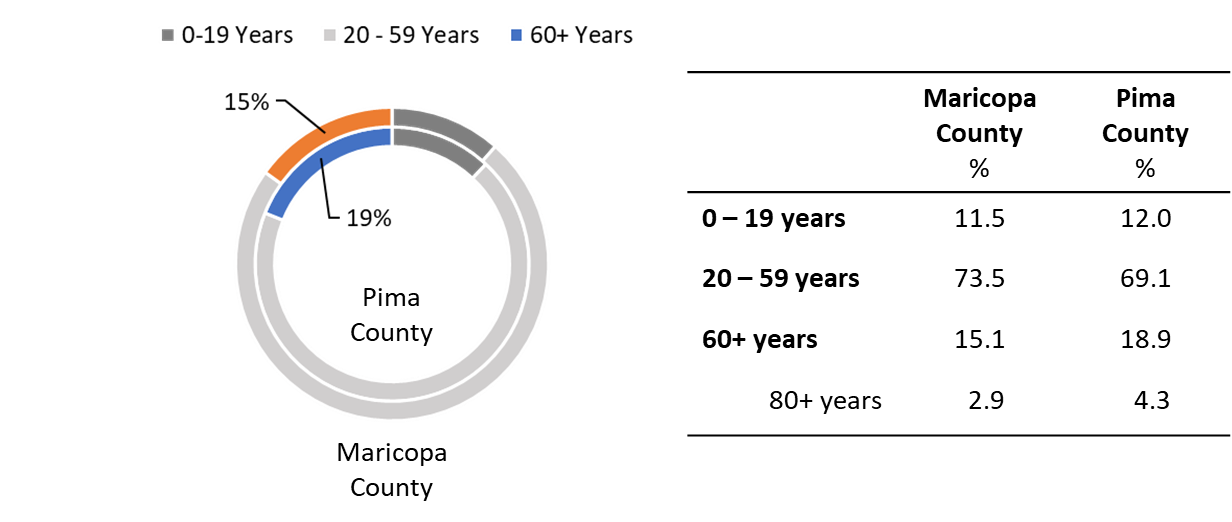
| Figure 2. Covid-19 Cases by Age in Maricopa County and Pima County through August 6, 2020. |
| Figure 3. Mean Age at Covid-19 Diagnosis in Maricopa County and Pima County March 15 through August 9. |
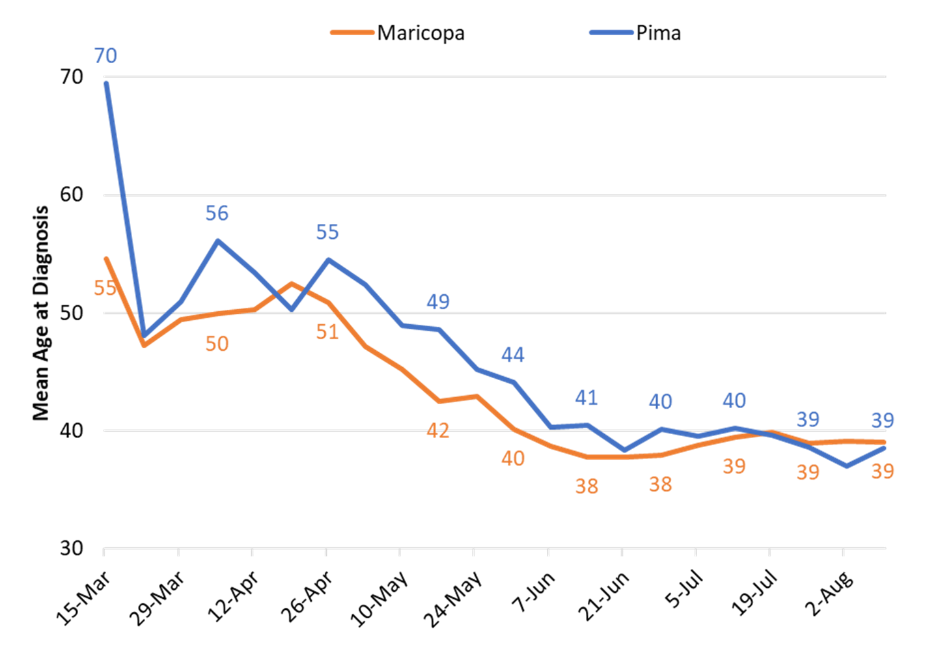
Between March 15 and July 5, the mean age at diagnosis was higher in Pima County than Maricopa County, 42.1 years versus 39.3 years, respectively. When the mean age at diagnosis is examined across the time course of the outbreak, the disparity in age was largest early in the outbreak and has since equalized (Figure 3).
When the distribution of cases by age is examined across time, two trends are apparent. First, Pima County has had a higher proportion of its diagnosed cases among those 60+ years of age than Maricopa County has (Figure 4). Second, the proportion of those diagnosed with Covid-19 who are 60+ years of age has fallen steadily in both counties over time.
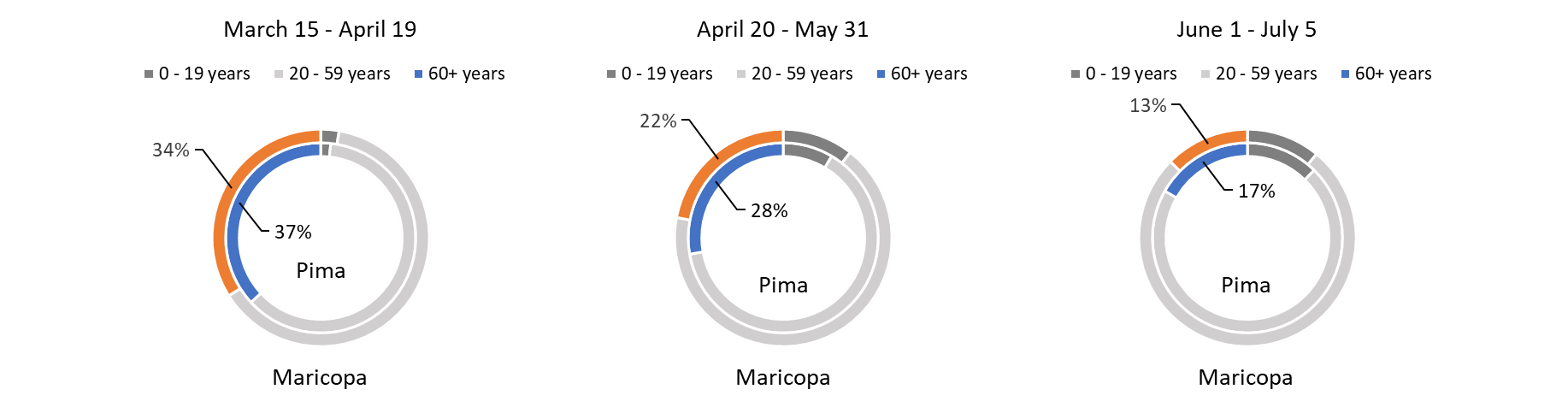
| Figure 4. Distribution of Covid-19 Cases by Age in Maricopa and Pima County through July 5, 2020. |
The county-specific crude CFR over 3 somewhat arbitrary time periods shows the largest differences early in the outbreak, between March 15 and April 19 (Table 2 and Figure 5 following page). The CFR for these analyses was calculated as the number of deaths occurring among cases diagnosed in a given week divided by the total number of cases during that week. Cases with no follow-up data were assumed to still be alive. Note: Unlike the CFR values reported in Table 1, those reported in Table 2 are lower because enough time has passed since July 5 to ensure the vast majority Covid-19 deaths were recorded. That is the principle reason why the subsequent analyses focus on the restricted time period between March 15 and July 5.
Table 2. Crude Covid-19 Case Fatality Ratio in Maricopa County and Pima County March 15 through July 5, 2020.
|
|
Mar 15 – Apr 19 (Period 1) |
Apr 20 – May 31 (Period 2) |
Jun 1 – Jul 5 (Period 3) |
Mar 15 – July 5 |
|
Maricopa County |
7.69% |
5.07% |
1.67% |
2.26% |
|
Deaths |
220 |
449 |
1142 |
1811 |
|
Cases |
2861 |
8861 |
68240 |
79962 |
|
Pima County |
12.78% |
6.30% |
2.16% |
3.73% |
|
Deaths |
129 |
119 |
192 |
440 |
|
Cases |
1009 |
1889 |
8896 |
11794 |
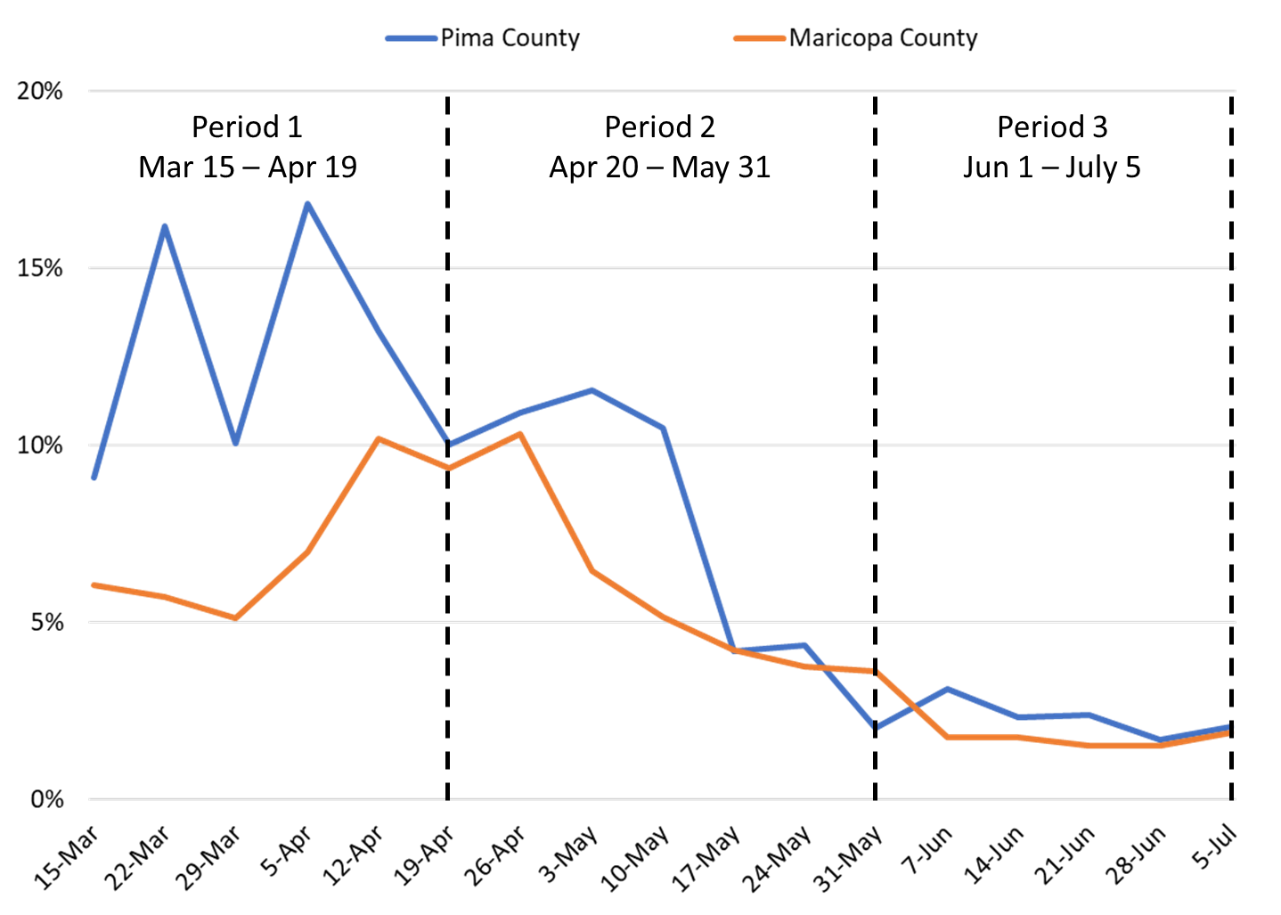
| Figure 5. Covid-19 Crude Case Fatality Ratio in Maricopa and Pima County March 15 through July 5, 2020. |
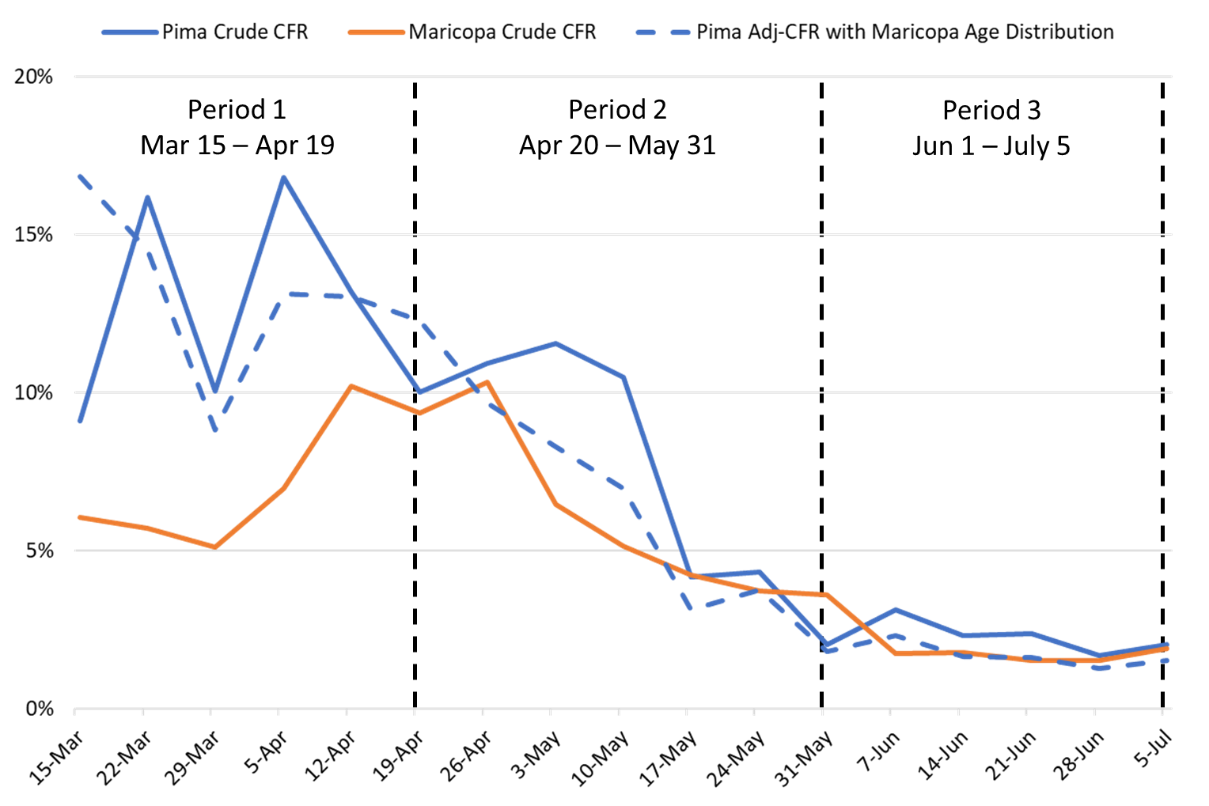
| Figure 6. Covid-19 Crude Case Fatality Ratio (CFR) in Maricopa County and Crude and Adjusted CFR in Pima County March 15 through July 5, 2020. |
The impact of differences in the age distributions can be accounted for by substituting Maricopa County’s age distribution of cases for Pima County’s age distribution while holding all other values constant. The results of this analysis are presented in Figure 6. If the age distribution of cases had been similar, then the respective CFRs would have been more similar as well. Note: Caution is warranted because of the small number cases and even smaller number of deaths prior to May 31, 2020. The values presented are overly precise and do not adequately reflect the inherent uncertainty.
When assuming equal distribution of cases across time by age in both counties, Pima County would have been expected to experience approximately 84 fewer deaths between March 15 and July 5. This would have reduced its CFR from 3.73% to 3.02% over the period eliminating about half of the absolute difference with Maricopa County’s 2.26% CFR. Therefore, differences in age distribution could have explained a considerable portion of the difference in CFR between the two counties. Because the early outbreak period represented a larger portion of Pima County’s outbreak, its higher CFR during the period has more impact on its overall CFR than the same period does for Maricopa County. Therefore, Pima County is likely to have a persistently higher overall CFR moving forward.
Table 3. Period Crude Covid-19 Case Fatality Ratio in Maricopa County and Adjusted Pima County Case Fatality Ratio after Equalizing Age Distribution, March 15 through July 5, 2020.
|
|
Mar 15 – Apr 19 (Period 1) |
Apr 20 – May 31 (Period 2) |
Jun 1 – Jul 5 (Period 3) |
Mar 15 – July 5 |
|
Maricopa County |
7.69% |
5.07% |
1.67% |
2.26% |
|
Deaths |
220 |
449 |
1142 |
1811 |
|
Cases |
2861 |
8861 |
68240 |
79962 |
|
Pima County (Obs) |
12.78% |
6.30% |
2.16% |
3.73% |
|
Deaths |
129 |
119 |
192 |
440 |
|
Cases |
1009 |
1889 |
8896 |
11794 |
|
Pima County (Adj) |
12.29% |
4.87% |
1.57% |
3.02% |
|
Deaths |
124 |
92 |
140 |
356 |
|
Cases |
1009 |
1889 |
8896 |
11794 |
Again, these results should be viewed cautiously, particularly the precision of the estimates as there were few cases and even fewer deaths, particularly early in the outbreak. Hopefully, others will examine this issue in due time with more robust statistical methods and greater access to other confounding variables. The primary value of this analysis is to recognize that similar attention should be given to “who is getting sick” as “how many are getting sick.”
While age is important as alluded to above, other important socioeconomic factors such as income, education, occupation, and family structure also influence the severity of Covid-19 disease among those infected. Any direct comparisons of crude Covid-19 mortality rates between geographic regions without accounting for age and other socioeconomic variables should be viewed cautiously.
Forecast reports to date, available as PDFs
Based on what we know now about this pandemic, we support guidelines for social distancing to slow the spread of the virus and urge everyone to follow the recommendations provided by the Centers for Disease Control and Prevention (CDC) to protect yourself, your family, your neighbors, and your employees. Please heed the recommendations as provided by the CDC, found at the following website: https://www.cdc.gov/coronavirus/2019-ncov/prepare/prevention.html
COVID covid coronavirus virus covid19 corona forecast model